We Offer Telemedicine Appointments.
Radiculopathy Pinched Nerve Treatments in Miami
Cervical, Thoracic and Lumbar Radiculopathy.
What is Radiculopathy?
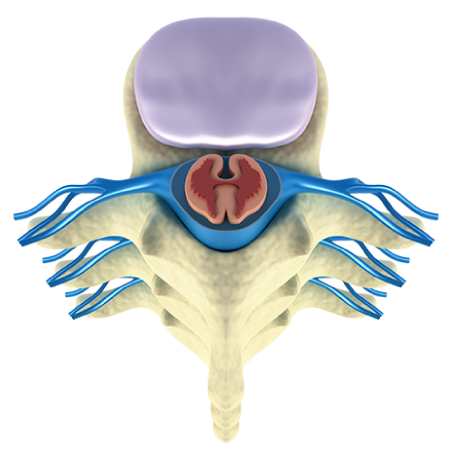
Radiculopathy is a common condition that involves a pinched nerve root within the spine. The spinal cord is a bundle of nerves that is encased in the spine. The nervous system is comprised of the central nervous system (the brain and spinal cord) and the peripheral nervous system (the nerve roots that branch off from the spinal cord into the rest of the body). The nervous system creates a network of signals throughout the body enabling sensation (sensory neurons) and movement (motor neurons). The spinal cord begins at the occipital bone at the base of the brain and runs through the cervical spine – the seven uppermost vertebrae – and then through the thoracic spine, which runs from the base of the neck to the abdomen. The lower section of the spine – the lumbar spine – contains the nerve roots which trail off from the spinal cord.
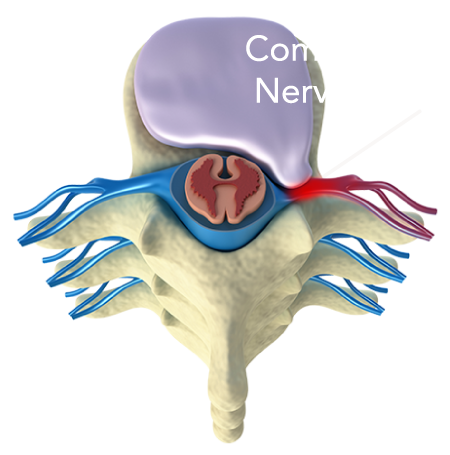
A pinched nerve is the result of excessive pressure on a nerve. This can be caused by surrounding bones, tissue, muscles or cartilage (intervertebral discs). The pressure disrupts the nerve functioning and causes the symptoms of radiculopathy. A pinched nerve can occur in several locations. For example, cervical radiculopathy involves a pinched nerve in the neck, while lumbar radiculopathy involves a pinched nerve in the lower back. Symptoms can usually be managed with medication, though in some cases, surgery may be required.
Radiculopathy
Healthy Disc
Herniated Disc
Types of Radiculopathy
There are several different types of radiculopathy. These include: Cervical Radiculopathy, Thoracic Radiculopathy and Lumbar Radiculopathy.
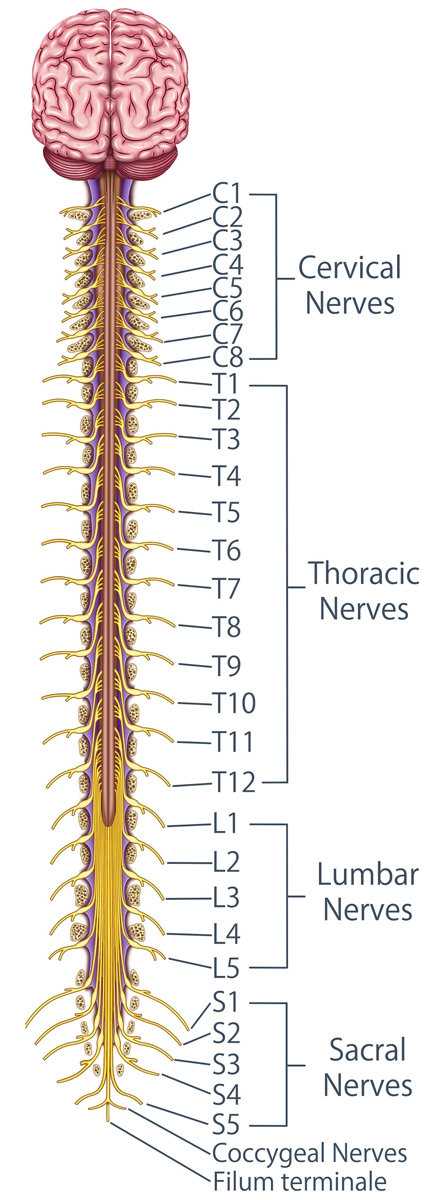
Cervical radiculopathy: This involves a pinched nerve in the neck (cervical spine) that becomes inflamed or damaged. This causes pain, weakness, numbness, or a tingling sensation in the neck that can radiate down to the shoulders, arms, and hands along the path of the nerves. The cervical spine contains eight pairs of nerve roots that branch of into the body. As they branch off from the spinal cord, the roots pass through the intervertebral foramen on each side of the spinal canal. The foramen is an opening between two vertebrae, and this is where the nerve may become compressed.
Thoracic radiculopathy: This involves a pinched nerve root in the central region of the spine (the chest/ upper back). It is less common than other forms of radiculopathy. The thoracic vertebrae have twelve pairs of spinal nerve roots passing through the foramen. If one of these nerves become inflamed or compressed it causes symptoms of thoracic radiculopathy: pain, numbness, and tingling in the ribs, side, and abdomen.
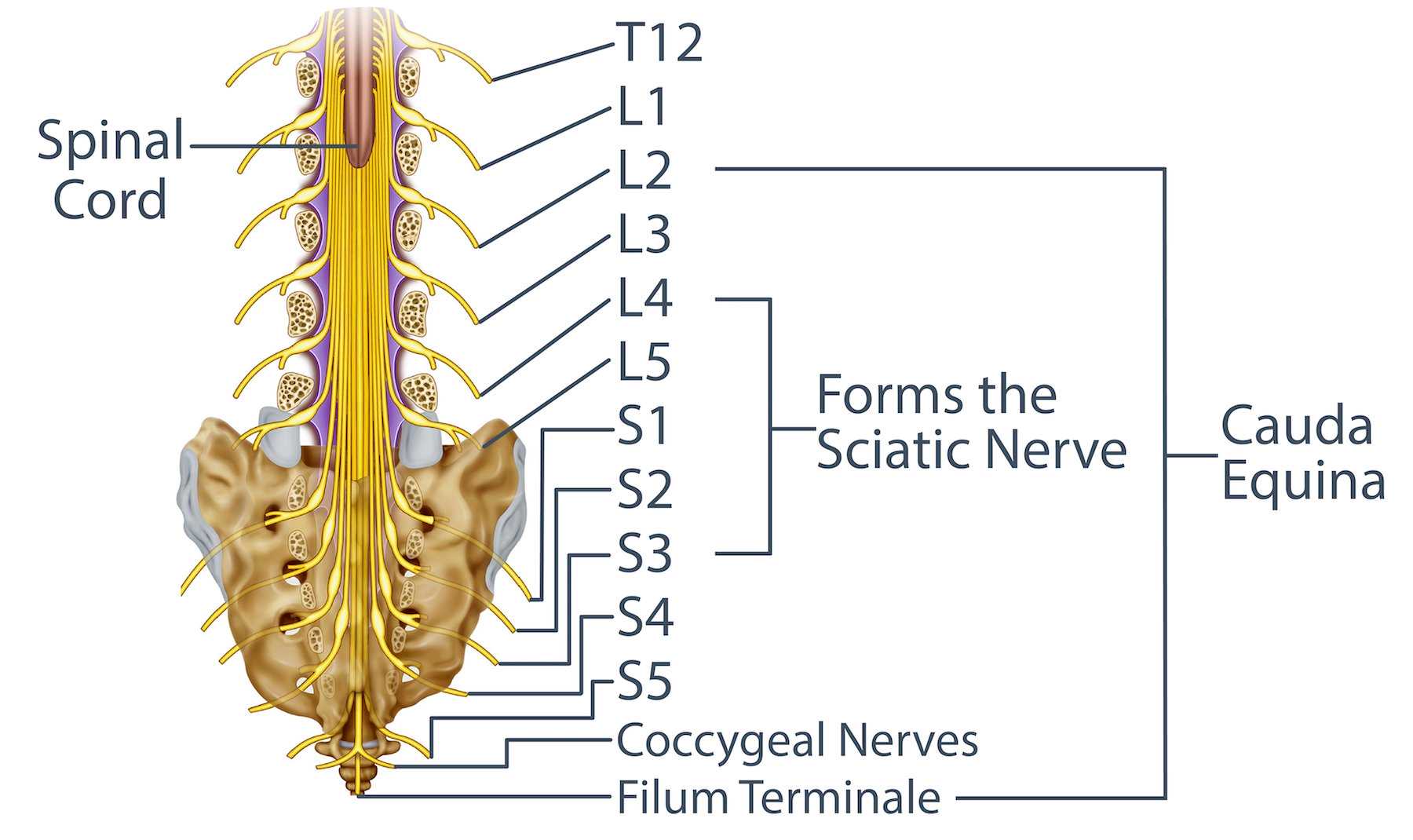
Lumbar radiculopathy: Also known as a pinched sciatic nerve, is caused by compression of a nerve root in the lower back. The spinal cord stops at the end of the thoracic spine and so does not run through the lumbar spine (see picture below). There are five nerve roots which pass into the lumbar region are known as the cauda equina because of their resemblance to a horse’s tail. When one of these nerve roots become compressed, it causes symptoms of lumbar radiculopathy.
The sciatic nerve is the long nerve which runs from the lower back and branches out into the hips, buttocks and down each leg. There is one sciatic nerve in each leg which is formed by the nerve roots branching out of L4, L5, S1, S2, and S3. When any of these nerves on either side of the spine become compressed or damaged it can cause burning or shooting pain down the sciatic nerve in the corresponding leg.
Spinal cord compression occurs when an injury or condition causes pressure on the spinal cord rather than a nerve root. It can occur in any region of the spine and may cause symptoms similar to those caused by radiculopathy.
Radiculopathy Symptoms
Cervical Radiculopathy Symptoms:
- Tingling
- Numbness
- Weakness
- Pain
These symptoms can occur in the neck, shoulders, arms, chest, and upper back.
Thoracic Radiculopathy Symptoms:
- A burning sensation
- Radiating pain
- Tingling
- Numbness
These symptoms can occur in the ribs, side, and abdomen. Thoracic radiculopathy is an uncommon condition and is sometimes misdiagnosed as a digestive disorder, a heart condition, a gallbladder complication, or shingles.
Lumbar Radiculopathy Symptoms:
- Pain in the lower back
- A sharp, burning, or tingling sensation that radiates down the leg
- Persistent pain in one buttock
- Buttocks and leg pain that worsens when sitting
- Difficulty standing due to pain
- Weakness or numbness in the foot
Causes of Radiculopathy
There are a number of different causes for cervical, thoracic and lumbar radiculopathy. These include:
Bone spurs: Also known as osteophytes, bone spurs can occur in the neck and back. They are the outgrowth of bones that form smooth protrusions along the edges of vertebrae. When this happens, they can put extra pressure on nerve roots. Bone spurs are caused by inflammation (such as osteoarthritis) and damage to cartilaginous intervertebral discs. They may also be caused by an injury that triggers bone growth to health the afflicted area.
Herniated discs: Each of the vertebrae is cushioned by a small round disc which is covered by a strong outer layer. The discs are located between each of the spinal column vertebrae and they protect the spine, hold the vertebrae together, and allow for movement of the spine. Also known as a ruptured disc, slipped disc, or disc extrusion, herniated discs occur when the cushioning center of one of the discs (the nucleus) pushes through the tough outer layer (the annulus). When this happens, it can irritate a local nerve, causing radiculopathy. A herniated disc can occur in any part of the spine but is most common in the lower back.
Degenerative disc disease: This is a condition that may arise with increasing age. It occurs when one or more of the discs between the vertebrae in the spine wears down and causes pain. Degenerative disc disease is a broad term for spinal conditions that are caused by the wearing down, drying out, or cracking of discs such as thinning discs, osteoarthritis, facet joint arthritis, herniated discs, bulging discs, or bone spurs. This term is not used to describe conditions that are caused by trauma or injury. These conditions can exert pressure on a nerve root, leading to radiculopathy.
Lumbar Spinal Stenosis: This is the narrowing of the spinal canal which is formed by the oval holes in each vertebrae that make up the spine. In a healthy spine, the spinal cord runs through the spinal canal absent surrounding pressure. However, when the spinal canal is narrowed due to osteoarthritis, bone spurs, trauma, damaged discs, tumors, and other spine diseases this can compress the spinal cord and nerve roots causing symptoms of radiculopathy.
Spondylolisthesis: This is when vertebrae slip over each other due to a break in the pars interarticularis (pars), which are the protruding segments of the vertebrae right before the facet joints on the inferior articular process. Spondylolisthesis can affect the pars on either side of the vertebrae. Prior to spondylolisthesis, there is a hairline crack or stress fracture in the pars that is called spondylosis. When a complete fracture occurs the spinal cord and nerve roots are constricted by the vertebrae shift causing lower back pain, radiating leg pain, and other symptoms.
Trauma: Radiculopathy may also be caused by trauma due to heavy lifting or a minor motorcycle or car accident.
Tumors: Spine tumors are tissue overgrowths that can occur inside the spinal cord (intramedullary tumors), outside the spinal cord but within the dura (intradural extramedullary tumors), or outside the spinal cord (extradural tumors) and cause pressure on the spinal cord and nerve roots.
Spine Tumors


Radiculopathy Risk Factors
Risk factors for developing radiculopathy include:
- Aging: the risk of radiculopathy increases with age.
- Excessive weight: being overweight puts extra strain on your spine.
- Lifting/posture: improper lifting and poor posture can put extra stress on the spine.
- Repetitive movements: repetitive movements such as frequent bending and lifting can put pressure on the spine.
Diagnosis of Radiculopathy
After discussing your medical history and your symptoms, our doctors will perform a physical examination. He or she may also test your reflexes and muscle strength to identify the affected nerve root. Our doctors may also order one of the following imaging tests:
- X-ray
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
You may also undergo a nerve conduction study, such as a Nerve Conduction Velocity (NCV) test. This test allows our doctor to assess if the affected nerve root is damaged. To take the test, you will remove any metal object, put on a gown, and sit or lie down on an exam table. After finding the affected nerve, our doctor will place two electrodes on your skin. After applying a mild electric pulse, your doctor will be able to record the level of stimulus between the two electrodes. You may feel mild discomfort but the test is not painful. The test may take between 10-20 minutes.
Radiculopathy Treatments
The type of radiculopathy treatment you receive will depend on the location of the pinched nerve, the underlying cause and the severity of the symptoms. Nonsurgical options are the first line of treatment. If these do not result in improvement after 6-12 weeks, our your doctor may consider surgical options.
Nonsurgical Treatments for Radiculopathy
Nonsurgical options include one or a combination of the following:
- Rest and posture: You should keep activity to a minimum./ You should avoid heavy lifting, going to the gym, and participating in sports activities. Maintaining a good posture while standing or sitting may also help.
- Physical therapy: Our doctor may refer you to a physical therapist who will be able to recommend stretching exercises which may relieve the pain.
- Heat and cold therapy: Alternating an ice pack and a heating pad to your neck or back may help relieve the pain. Apply each for fifteen minutes with a 2-3 hour period in between.
- Over-the-counter medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended for treatment of cervical, thoracic and lumbar radiculopathy. Examples of NSAIDs include ibuprofen and aspirin.
- Epidural steroid injections: Once your doctor has located the affected nerve root, he or she may administer an epidural steroid injection. The procedure involves the use of a fluoroscope (an X-ray imaging technique) and contrast dye to guide the injection into the right spot. This will help to relieve the pain.
- Cervical collar: In the case of cervical radiculopathy, if you are suffering from severe neck pain, your doctor may recommend a cervical collar for up to a week. Wearing the device will help to keep your neck immobilized, which may help to reduce inflammation.
Surgical Options for the Treatment of Radiculopathy
The aim of surgery is to relieve nerve compression, restore mobility, and relieve pain. There are several different surgical procedures which may be used, depending on the location of the pinched nerve and the underlying cause. Surgical options include:
Microdiscectomy: This surgical procedure can be used to relieve the symptoms of lumbar radiculopathy caused by a herniated disc. This procedure involves the removal of a small piece of the disc from the area where the nerve root is being compressed. This allows the root more room so it can heal.
Prior to this procedure, you will be given a general anesthetic. The surgeon will make a small incision in your back above the affected vertebra. After moving the muscle, the surgeon will remove a small piece of vertebral bone for surgical access to the disc. The damaged herniated disc and surrounding tissue will then be removed, decompressing the nerve. The incision will then be sutured.
You should be able to return home within 24 hours. You should avoid heavy lifting or strenuous exercise and should be fully recovered after six weeks.

Laminectomy
This type of surgery involves the removal of the entire lamina, which includes the laminae on both sides of the vertebra and the spinous process. The lamina is the layer of a vertebra bone that forms the posterior (back facing) wall of the spinal canal. Removing the lamina enlarges the spinal canal and decompresses the pinched nerve root.
For this procedure you will be given a general anesthetic. The surgeon will make a small incision in your back above the affected area. After moving the muscle aside, the surgeon will remove the lamina and then suture the incision. You may have a brief hospital stay after the surgery. You should be able to return to work within a few weeks.

Laminoplasty
This surgical procedure enlarges the spinal canal by removing one of the laminae on either side of the vertebra, hinging the remaining lamina structure open like a door (open-door technique), and inserting a sturdy device on top of the vertebra that functions as an elongated laminae holding the remaining bone in place.

Laminotomy
This is a surgical procedure to remove a portion of the laminae from the affected vertebra. The aim of the surgery is to relieve pressure from a pinched nerve root.
Prior to this procedure, you will be given a general anesthetic. The surgeon will make a small incision above the vertebra to be treated. After moving the muscle tissue, the surgeon will remove a small amount of bone from the laminae (the layer of a vertebra bone that forms the wall of the spinal canal). The incision is then closed and sutured.
You should be able to return home within 24 hours after the surgery. You should be able to return to work within a few weeks.

Hemilaminotomy
This procedure is like a laminotomy except the surgeon removes a portion of the laminae only on the side of the vertebra where the nerve decompression is needed.

Foraminotomy
This is a surgical procedure which is performed to widen the area around the foramen which is compressing a nerve root. The foramen are the circular archways on either side of two adjacent level vertebrae through which the nerve roots thread from the spinal cord, branching into the rest of the body. The aim of the surgery is to relieve pressure on the pinched nerve.
You will be sedated during this procedure using a general anesthetic. The surgeon will make a small incision above the vertebra to be treated. After dissecting the muscle tissue, the surgeon will remove a small amount of bone inside the foramen. The incision is then closed and sutured.
You should be able to return home within 48 hours. Your doctor will advise you of any movements you need to avoid. You should be able to do light work after a few weeks and heavier work within a few months.
At Miami Neouroscience Center we help patients with Radiculopathy or pinched nerve symptoms using the latest techiques and treatments, contact us today (786) 871-6856.
Radiculopathy Recovery
It can take a couple of weeks before you will begin to feel better. You can help your recovery with the following:
- Rest: Getting plenty of rest will help to take the strain off your spine and promote healing. You should avoid heavy lifting, strenuous exercise, and repetitive movements during your rehabilitation.
- Physical therapy: In some cases, physical therapy may be beneficial. For example, in the case of lumbar radiculopathy, lumbar traction may be used. Lumbar traction involves gently stretching and manipulating the back using weights, devices, or therapeutic applied force. This opens the spaces between the vertebrae, alleviating pressure. This can provide temporary pain relief.
- Massage: Gentle massage around the affected area can help to relieve pressure. A full body massage can also ease tension and help you to relax. However, you should avoid deep tissue massage as this could worsen radiculopathy.
- Laser therapy treatments: Also known as cold laser therapy, this treatment involves the application of low-intensity, focused laser light. When applied directly to the affected area it can promote healing and relieve pain. Laser therapy may also help to heal damaged nerves.
Radiculopathy Prevention
You can reduce your risk of radiculopathy by:
- Maintaining a healthy weight
- Staying physically fit
- Maintaining good posture
- Using kinetic lifting which involves proper body positioning:
- Keeping a wide stance when lifting
- Squatting to lift with your legs and not your back
- Keeping a straight/ concave spine not convex
- Smooth movements (no quick/ jerking movements)
FAQ - Frequently Asked Questions
The most common cause of this condition is a herniated disc.
Lumbar radiculopathy is the most common form of this condition with around 83 cases per 100,000 people.
Radiculopathy involves the compression of a nerve root, whereas myelopathy involves the compression of the spinal cord.
With rest and the proper treatment, most people with a pinched nerve in the neck or back will begin to feel much better within a week or two. Complete healing can take up to three months.
Piriformis syndrome is when a muscle in the buttocks (the piriformis muscle) compresses the sciatic nerve, which runs from your hip down your leg. In contrast, lumbar radiculopathy is when the nerve roots in the lumbar spine are compressed. Both of these diagnoses can cause symptoms of sciatica including tingling, shooting, numbing, radiating, or burning pain from the buttock into the leg and foot, however the root cause is different: muscle vs nerve root.
There is one sciatic nerve on each side of the body that is formed in the pelvis from the nerve roots L4 through S3. The sciatic nerve exits the greater sciatic foramen and most commonly runs below the piriformis muscle (Type I - Undivided). However, variants can occur including Type II through Type VI.
- Type II - the nerve runs through and below the piriformis muscle
- Type III - the nerve runs above and below the piriformis muscle
- Type IV - the nerve through the piriformis muscle
- Type V - the nerve runs through and above the piriformis muscle
- Type VI - the nerve runs above the piriformis muscle
When the piriformis muscle pinches the sciatic nerve this can cause symptoms of sciatica. Piriformis syndrome can occur from muscle spasms, injuries, irritation, tightening, and inflammation.
Yes, and often it can be treated without surgery.
Finding a pinched nerve specialist in Miami would first involve a diagnosis by usually a primary care physician or neurologist, then they will refer you to a neurosurgeon that will treat the condition, Dr. Mouw is an experienced neurosurgeon that can treat and diagnose Radiculopathy.
Resources
Thomas Scioscia, MD, "Spinal Cord and Spinal Nerve Roots" SPINE-health, August 2017. https://www.spine-health.com/conditions/spine-anatomy/spinal-cord-and-spinal-nerve-roots
Lee Dubay, "Low-level laser therapy is promising as neuropathic pain treatment" BioOptics WORLD, April 2017. https://www.bioopticsworld.com/biomedicine/article/16433852/lowlevel-laser-therapy-is-promising-as-neuropathic-pain-treatment
Physiopedia, "Lumbar Radiculopathy". https://www.physio-pedia.com/Lumbar_Radiculopathy
Brittney A. Giuffre; Rebecca Jeanmonod, "Anatomy, Sciatic Nerve" NCBI, December 2018. https://www.ncbi.nlm.nih.gov/books/NBK482431/
To see if you have a pinched nerve and to learn more about your treatment options please call us at 786.871.6856 or schedule a consultation today!